A 42 year old homemaker, mother of 2, sustained a closed fracture of the radius ulna in February 2011.
She saw an orthopedic surgeon close to her home, and an open reduction and internal fixation by plates was done on the same day.
 |
| Immediate Postoperative Xray |
The Antibiotic was changed - presumably, a higher antibiotic was administered.
This settled the fever somewhat, but the woulnd was noted to be 'gaping'. This was secondarily sutured on the 5th day and she was sent home.
However, the patient continued to be 'ill' and had pain & swelling in the operated limb, and decided to take a second opinion.
The second surgeon removed the radial plate and put on an external fixator on the radius.
The ulnar plate was retained.
 |
| Radial plate removed and Fixator applied |
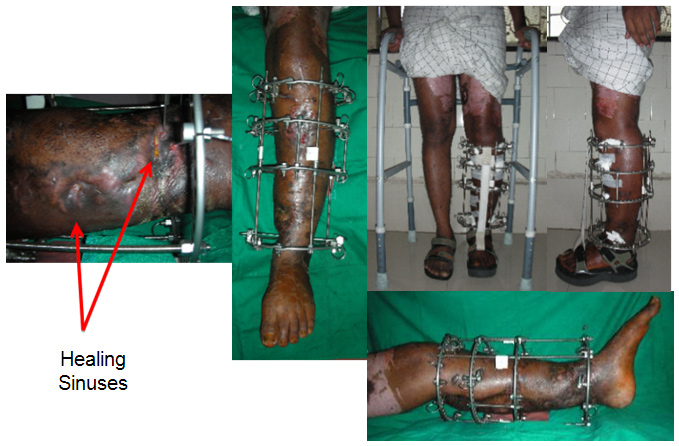
She continued to be troubled by discharge from the radial incision and another 3 weeks later the ulnar incision began discharging seropurulent fluid.
This was tackled by removal of the ulnar plate and application of a fixator.
 |
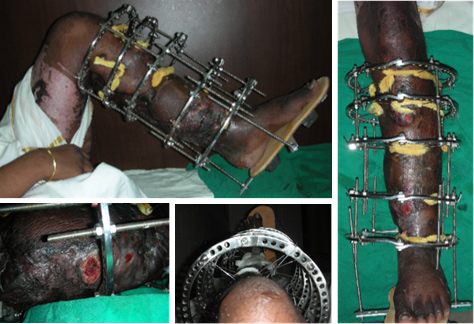
| Ulnar plate removed and fixator applied |
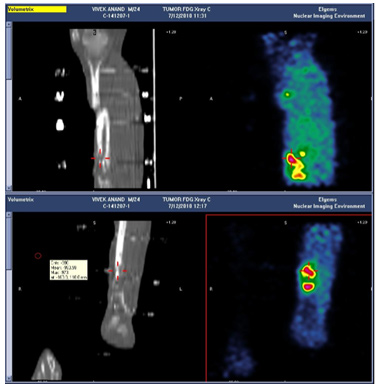
She was asked to get a scan done, and when she came to the scan center which is in the same building she apparently saw the CLLR board which specifically lists infection/osteomyelitis as one of our areas of expertise, and has a line "Cutting edge techniques tempered by 25 years of experience".
That prompted her to seek our opinion.
 |
| Pinsites get worse, Radius sequestrating |
 |
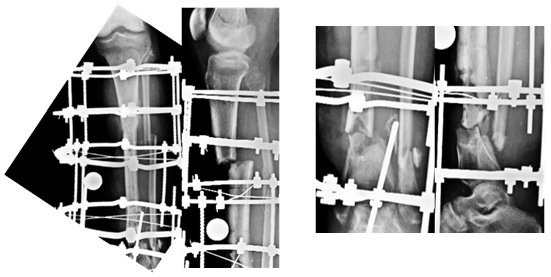
| X-ray at presentation |
After reviewing her history, reviewing her xrays and examining her, we sat her down (along with husband and a couple of relatives) and discussed the options before her.
 |
| Clinical Appearance and pinsites at presentation |
She seemed to have a 'wrist drop' which I thought was more because of adhesions or the inflamation within the compartment, rather than a problem with the radial or posterior interosseous nerve.
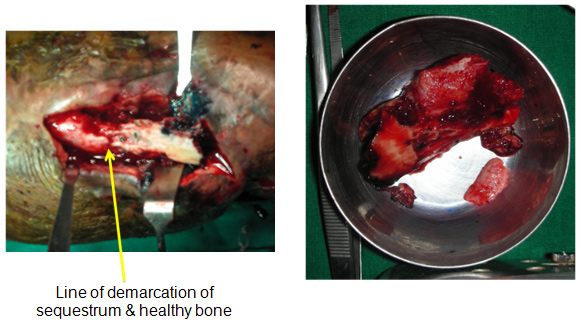
The only option really in my opinion was to do a proper debridement, clear the infection and then think of the reconstructive aspect.
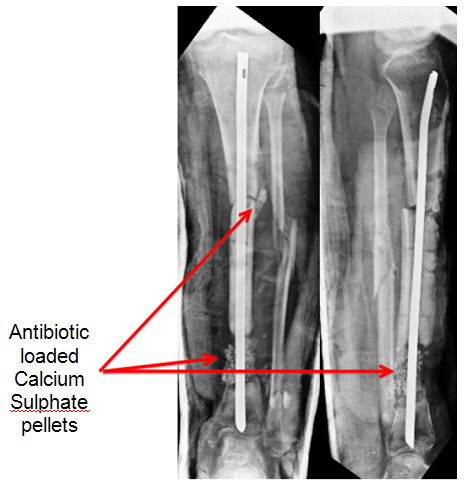
In May 2011, we did the surgery for her and the plan was to do a thorough debridement, use local antibiotic in Calcium Sulphate pellets (Stimulan), and stabilise.
The debridement and the antibiotic pellets was the 'easy' part. How to stabilise a large defect (for I was pretty sure that was what we were going to have at the end of debridement.
 |
| Central diaphysis of the Radius and Ulna sequestrated |
Also, having had a fair amount of experience with the TENS nail, I was certain of a reasonable stability as long as the right size and right length (to seat it well upto subchondral bone) was used.
We put in the nails and took care to seat the ends as close to the subchondral bone as we could, thereby gaining some rotational stability. At the lower end of the radius, I buried the end into the bone to provide some resistance against collapse.
Surprisingly (maybe not so surprisingly), with the nails in the forearm was quite stable, to rotation and also preventing collapse of the gap.
We filled in the empty space with Stimulan loaded with 2 gms vancomycin and 3 million units Colistin (based on the earlier culture reports) and sent off tissue samples from multiple areas in the wound for culture (which would decide our IV antibiotics.
 |
| Stabiised by TENS nail. Stimulan Pellets for local Antibiotic Delivery |
 |
| Incisions 2 days and 7 days after surgery |
I have been minimising the use of IV antibiotics based on a combination of clinical appearance and response, and blood parameters - notably CRP. Based on these, we stopped IV antibiotics after 3 weeks, despite the CRP not being normal, but it was showing a clear downward trend and the patient was comfortable.
No further antibiotics were administered to her after this.
 |
| Healing of the Incisions |
The TENS nails did their job of stabilisation well, and xrays showed gradual disappearance of the pellets (as expected).
 |
| Pellets Dissapear over time. TENS nail holds position well |
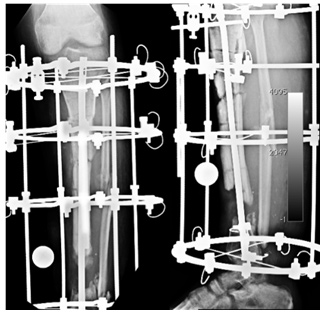
Our plastic surgeons were happy to do a double barreled fibula, and we fixed it with a long titanium plate that almost covered the bones completely.
 |
| Vascularised Fibula with Pedicle, Plate fixation thru single incision |
 |
| Vascularised Fibula with Skin paddle |
 |
| Double Barrelled Fibula and LCP fixation |
 |
| Excellent Function, except for pronation beyond midprone |
 |
| Solidly Healed on Xray |
1. the recognition of the destructiveness of infection,
2. of the need for experience to deal with it aggressively,
3. of the requirement of the surgeon to deal with the surgery, the pharmacology and the psychology of infection.
4. the need to use the best knowledge, techniques, and tools/implants available to achieve an optimal result.